Liver and pancreas are vital organs in the digestive system. The abnormalities of liver and pancreas are usually susceptible to develop further serious diseases due to their complicated structures and functions. Disorders of the liver and pancreas can range from mildly troublesome to intensely painful. It might start from acute to chronic inflammation and infection, benign hepatic or pancreatic tumor and hepatic cysts as well as liver and pancreatic cancers.
It is widely acknowledged that alcohol abuse or alcoholism is one of the major contributing factors to develop acute and chronic inflammation of both liver and pancreas. Fatal conditions caused by alcoholic abuse include a severely liver inflammation, acute liver failure or/and cirrhosis presented with liver cancer. Besides serious conditions of liver and pancreas, other body’s systems are substantially impacted including digestive system, cardiovascular system, endocrine system, kidney, blood circulation and coagulation process as well as impaired immune system which subsequently leads to severe infection and sepsis. These health conditions largely disrupt the quality of life, both physically and mentally. Early diagnosis and timely treatment result in decreased disease severity and reduced mortality rates.
Liver diseases
Liver disease or hepatic disease is any disturbance of liver function that causes illness. Liver disease can be induced by a wide range of causes. Nevertheless, primary causes of liver disease include:
- Alcohol abuse:
Liver diseases such as cirrhosis and liver cancer are prone to happen in men rather than women with particular contributing risk factors including heavy or chronic alcohol use. Over time, damage to the liver results in scarring (cirrhosis) which can eventually lead to liver failure and liver cancer. The chances of developing disease are largely determined by the amount of alcohol intake and duration. In case of high amount of alcohol consumption in a 2-week time, liver fatty might potentially develop. Chances of cirrhosis significantly increase if the duration of alcohol consumption is longer than 5 years, with amount of alcohol 20-30 grams/ day in women or 40-50 grams/ day in men. Effects of alcohol on individuals might widely vary depending on amount of alcohol intake, drinking pattern e.g. drinking on empty stomach without food and other personal factors. Chronic and excessive alcohol consumption produces a broad spectrum of hepatic lesions, the most characteristic of which are fatty liver (steatosis), hepatitis, cirrhosis, liver failure and liver cancer. After digestion process, alcohol and its metabolic byproducts, including acetaldehyde, contribute to liver injury by causing liver cell damages. As a result, liver cannot function normally, leading to an accumulation of fat in the liver, known as fatty liver. Furthermore, liver injury leads to inflammation in alcoholic hepatitis through a classical sterile necrosis response. In fact, if alcohol consumption is discontinued during the early stage of liver damages, the liver will be able to compensate for its limited function. At the end, liver function can be fully preserved. However, if alcohol consumption continually persists, the self-compensation mechanism of the liver eventually fails. Liver damages from repeated and excessive alcohol abuse results in fibrotic scars, alcoholic liver cirrhosis, liver failure and eventually end-stage liver cancer.
- Genetics:
Abnormal genes inherited from the parents can cause various abnormal substances in the liver. Genetic abnormality also causes the deficiency of certain liver enzyme (Alpha-1 antitrypsin). These result in liver damages or malfunctions, leading to impaired liver functions, cirrhosis and liver cancer.
- Certain underlying diseases, hematological disorders and hepatitis B and C infection:
Accompanied with alcohol abuse, these conditions rapidly progress and eventually turn to cirrhosis and liver cancer.
- Exposure to carcinogenic substances that induce liver cancer:
Carcinogenic substances include certain foods contaminated with afla-toxin such as groundnuts, tree nuts and maize, grilled or over-burnt meats that contain heterocyclic amines (HCA) and polycyclic aromatic hydrocarbons (PAH), processed foods with potassium nitrate and uncooked freshwater fish containing liver flukes that potentially cause cholangiocarcinoma, an aggressive cancer arising from epithelial cells of the bile duct.
- Cigarette smoking:
Tobacco smoking is one of the major risk factors for several chronic diseases. Several studies indicate that smoking is also strongly associated with liver diseases such as neoplasm of liver and chronic liver disease.
- Taking some medications, herbal supplements or toxic chemicals:
Certain medications have profound side effects to the liver such as paracetamol overdose. Herbal supplements with unknown quantity and quality of active ingredients must be avoided since these substances might damage the liver, leading to fatal conditions such as acute liver failure.
Warning signs and symptoms of liver disease
Typically, liver disease does not produce any specific signs and symptoms until disease progresses to advanced stages. Relevant symptoms that might indicate liver abnormalities include loss of appetite, unintentional weight loss, bloating or flatulence and chronic constipation. Patients might experience abdominal pain in the upper right abdomen where liver locates. If disease continues to progress, specific symptoms are ascites due to the abnormal buildup of fluid in the abdomen and dark urine color which is unsolved even after loading water as well as jaundice, a yellow discoloration of the skin and the whites of the eyes.
Diagnosis of liver disease
Annual heath check-ups remain essential in order to screen warning symptoms at early stage. To diagnose liver disease, doctors perform full physical investigations including medical history taking e.g. presenting signs and symptoms and family history as well as physical examinations and additional imaging tests if necessary. Fatty liver is one of the most common liver diseases found in patients with risk factors e.g. being obese or overweight, diabetes, high blood pressure, high triglyceride levels and alcohol consumption. The best possible way to prevent alcohol-induced liver disease is to stop drinking which allows hepatic cells to restore the capacity to regenerate and function. If risk factors remain, acute hepatitis might turn to be cirrhosis, a late stage of scarring (fibrosis) of the liver and eventually cause liver cancer.
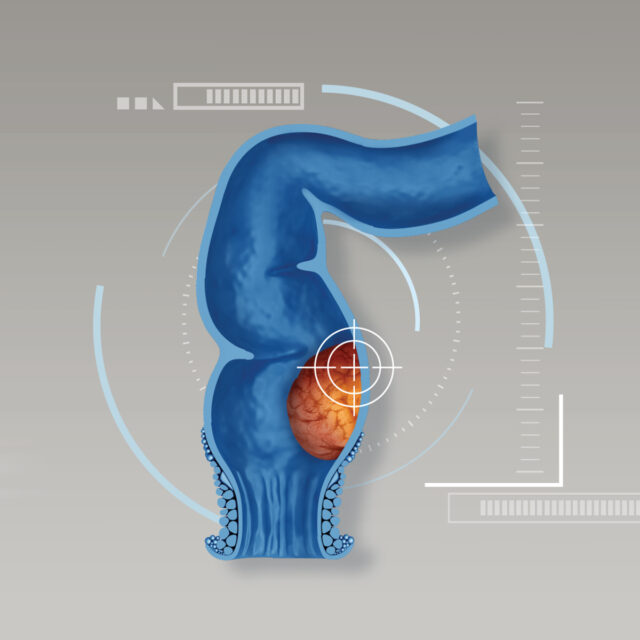
Pancreatitis
The pancreas is a long, flat gland that locates behind the stomach in the upper abdomen next to the beginning of small intestine. The pancreas produces enzymes that help digestion (carbohydrates, proteins and fat) and hormone, insulin that regulates blood sugar level (glucose).
Pancreatitis is an inflammation in the pancreas which occurs when the digestive enzymes are activated before they are released into the small intestine and these enzymes begin attacking the pancreas and causing inflammation. There are two forms of pancreatitis: acute and chronic. Acute pancreatitis appears suddenly and normally lasts for days while chronic pancreatitis occurs over many years.
1) Acute pancreatitis:
Acute pancreatitis suddenly happens and it normally lasts for days. Contributing factors to acute pancreatitis mainly involve:
- Gallstones: Gallstones, produced in the gallbladder, can block the bile duct, stopping pancreatic enzymes from traveling to the small intestine and forcing them back into the pancreas. The enzymes then begin to irritate the cells of the pancreas, causing the inflammation associated with pancreatitis.
- Chronic alcohol abuse: After alcohol digestion process, alcohol and its metabolic byproducts, including acetaldehyde, contribute to liver injury by causing liver cell damages. Chronic and excessive alcohol consumption produces a wide spectrum of hepatic lesions, the most characteristic of which are fatty liver (steatosis), hepatitis, cirrhosis, liver failure and liver cancer. In addition, long-term consumption of alcohol results in calcified pancreas and fibrotic tissue that eventually induces chronic pancreatitis.
Symptoms of acute pancreatitis:
Signs and symptoms of pancreatitis may vary, depending on its severity. Presenting symptoms are upper abdominal pain that might radiate to the back, abdominal tenderness, loss of appetite, nausea and vomiting. Food usually worsens symptoms. Severe abdominal pain might disrupt sleep.
Diagnosis of acute pancreatitis:
Tests and procedures used to diagnose acute pancreatitis include:
- Medical history taking with the history of alcohol consumption. If there is the presence of long-term alcohol use, alcohol-induced acute pancreatitis is primarily suspected.
- Physical examination
- Blood tests to determine CBC (complete blood count), levels of pancreatic enzymes and other related components.
- Serum amylase and lipase levels. These enzymes are typically elevated in patients with acute pancreatitis.
- Abdominal ultrasound to identify gallstones and pancreatic inflammation. In addition, endoscopic ultrasound might be used to evaluate inflammation and blockages in the pancreatic duct or bile duct.
- Other tests might include Computerized tomography (CT) scan and Endoscopic retrograde cholangiopancreatography (ERCP).
Treatment of acute pancreatitis:
Treatment options for acute pancreatitis depend on symptoms and disease severity. Dehydration and shock may occur. Treatments include intravenous (IV) fluids, as the body devotes energy and fluids to repair inflamed pancreas, pain medications and close monitoring of possible complications. In addition, treatment will be selected based on the causes of inflammation. If pancreatitis caused by gallstones, surgery to remove gallbladder is further recommended. Pancreas surgery may be necessary to drain fluid from the infected pancreas or to remove dead tissue. If left untreated, complications might develop and lead to increased chances of death
2) Chronic pancreatitis:
Major contributing factor of chronic pancreatitis is long-term alcohol abuse which causes liver damages repeatedly over a prolonged period of time, resulting in chronic inflammation of pancreas.
Symptoms of chronic pancreatitis:
Signs and symptoms of chronic pancreatitis are considerably similar to acute episode. Main symptom is severe upper abdominal pain which often radiates to the back and usually gets worse and cannot be relieved after taking medicines. Nonetheless, some patients might not exhibit abdominal pain. Since a damaged pancreas cannot produce digestive enzymes, patient with chronic pancreatitis may develop problems with digesting and absorbing food and nutrients. This can lead to weight loss, vitamin deficiencies, diarrhea and greasy, foul-smelling stools. Over time, a damaged pancreas also can fail to produce sufficient insulin, which results in high blood sugar level. Additionally, patients diagnosed with chronic pancreatitis have a greater chance of pancreatic cancer.
Effective treatment of liver and pancreatic diseases
To treat liver and pancreatic diseases effectively, alcohol discontinuation is highly recommended in order to allow hepatic cells to restore the capacity to regenerate and function, therefore disease progression can be delayed. Treatment options to treat liver, pancreatic and biliary diseases include:
- Targeted therapy which results in decreased mortality rates and reduced serious complications
- Sufficient intravenous fluid replacement and other medications and vitamins.
- Surgical treatments which include conventional surgery (open surgery) and minimally invasive surgery (MIS)
- Interventional treatments
- Liver transplant in patients who failed to previous non-surgical treatments
In case that pancreatitis is diagnosed with the presence of local complications such as necrotizing pancreatitis, defined as a condition where parts of the pancreas die due to lack of sufficient blood supply and may get infected, surgery may be necessary to drain fluid from the infected pancreas or to remove dead tissue (pancreatic necrosectomy). Surgical removal of either whole pancreas or only affected part of the pancreas is considered effective treatment option in patients who have pancreatic cancer without the metastatic evidences to other organs in the body.
Taking good care of liver, pancreas and bile ducts
Regular health check-ups and early diagnosis substantially result in effective and timely treatments, leading to decreased disease severity and lowered chance of developing serious complications. To strengthen liver, pancreas and biliary system, recommendations may include:
- Stop alcohol drinking;
- Consume healthy foods with appropriate amount;
- Avoid eating high-fatty diets;
- Use clean spoon to prevent transmission of hepatitis virus;
- Take beneficial supplements under supervision of the experts;
- Exercise regularly;
- Have regular health check-ups at least every year; and
- Receive vaccination against hepatitis A and B infection.
If gallstones are found, urgent treatment must be provided. Being aware of warning signs and symptoms remains essential. If abnormal signs exhibit, medical attention must be sought as soon as possible in order to receive accurate diagnosis and appropriate treatments.