Diabetes mellitus is among the most common chronic diseases affecting people’s health across the world. Globally, the numbers of people with diabetes have been currently rising to more than 300 million. Particularly in Thailand, the estimated number of diabetic patients is considerably high, up to 3.2 million. This amount, as national prevalence of diabetes, represents 6.4{6bcfa6d34ef78e64a6611219045b248162a175f846eea5cbdfd8429a6e545bd3} of Thai adults. Due to lack of disease awareness in conjunction with poor disease management, the prevalence of diabetes appears to substantially increase worldwide. The longer the patients have diabetes and the less controlled blood sugar, the higher the risk of diabetes-related complications.
Diabetes mellitus
Diabetes mellitus, commonly known as diabetes, is defined as a metabolic disease that leads to high blood sugar. In normal condition, insulin as a crucial hormone lowers the amount of sugar in the blood circulation by moving sugar from the blood into the cells to be stored or used for energy. With diabetes, the body either does not produce sufficient amount of insulin or cannot use insulin effectively due to insulin resistance. Instead of being transported into the cells, sugar builds up in the bloodstream, causing high blood sugar. Overtime, regardless of the type of diabetes, uncontrolled blood sugar can potentially cause a wide range of diabetes complications which may be disabling or even life-threatening, such as cardiovascular disease, kidney damage (diabetic nephropathy) and nerve damage (diabetic neuropathy) as well as eye damage, known as diabetic retinopathy.
Get to know diabetic retinopathy
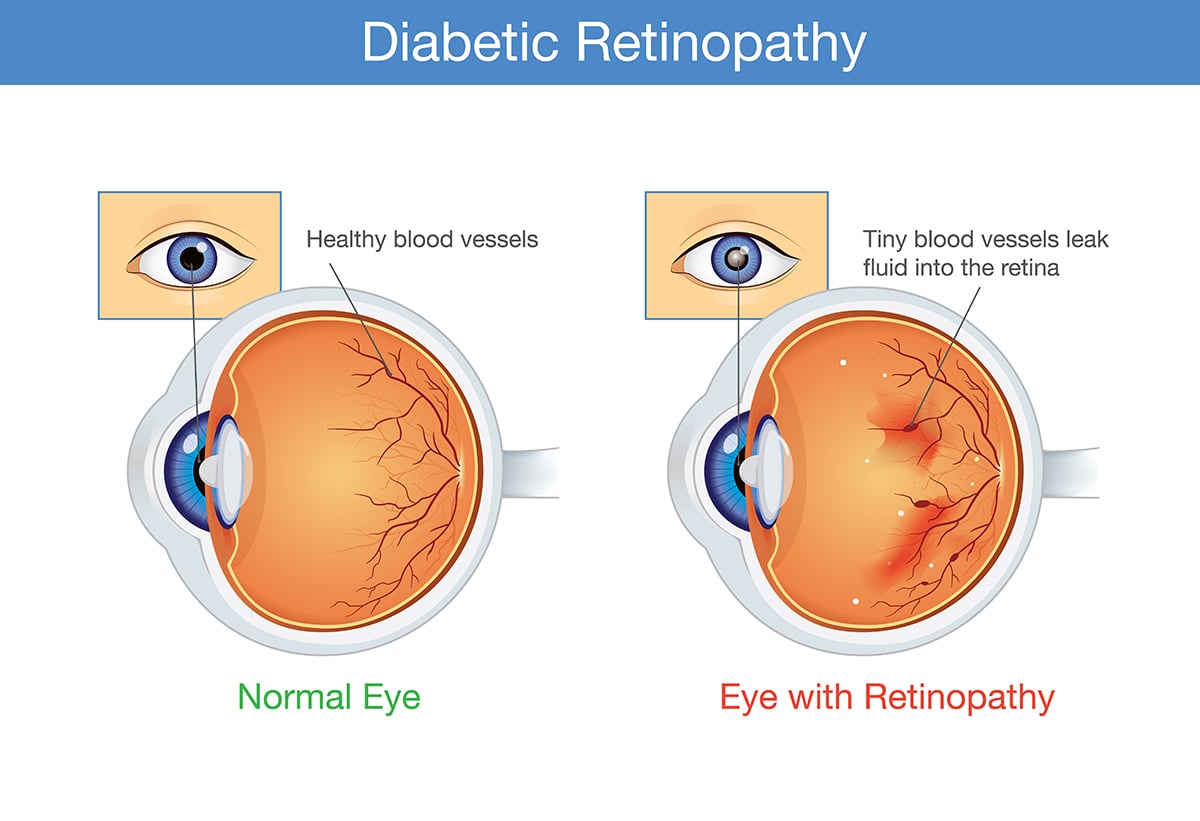
Diabetic retinopathy is a complication of diabetes, caused due to prolonged high blood sugar levels damaging the back of the eye or retina, an essential part of the eye that enables vision. It can eventually cause blindness if left undiagnosed or untreated. In addition, diabetes also increases the risk of other serious vision problems, such as glaucoma and cataracts.
Stages of diabetic retinopathy
Diabetic retinopathy involves the growth of abnormal blood vessels in the retina. Over time, excessive sugar in the blood can cause the blockage of the tiny blood vessels that nourish the retina, resulting in cutting off its blood supply. To naturally compensate, the eye attempts to grow new blood vessels. However, these new blood vessels do not develop properly, leading some undesired consequences on the retina. Regarding disease severity, there are two types of diabetic retinopathy:
- Nonproliferative diabetic retinopathy (NPDR): During early stage of diabetic retinopathy, the walls of blood vessels in the retina are weakened. Tiny bulges in the blood vessels, known as microaneurysms, protrude from the walls of the smaller vessels and may leak fluid and blood into the retina. This leakage can cause swelling of the macula, the center portion of the retina. Meanwhile, larger retinal vessels can begin to dilate and become irregular in size. The condition can progress from mild without noticeable signs and symptoms to severe as more blood vessels become blocked. In some cases, retinal blood vessel damages might lead to a buildup of fluid or edema in the macula. If macular edema develops, it often causes impaired vision. In case of severe blockage or occlusion, muscular ischemia can further exhibit, potentially leading to complete vision loss.
- Proliferative diabetic retinopathy (PDR): As an advanced form of diabetic retinopathy, damaged blood vessels become completely occluded, causing the growth of abnormal blood vessels in the retina. These newly formed blood vessels are fragile and susceptible to leak into vitreous –the jellylike substance that fills the center of the eye. Eventually, scar tissue, as the result of the growth of these new blood vessels, can cause the retina to detach from the back of the eye. Retinal detachment affects vision by causing blurred vision or darkness or curtain-like images in the vision. If not treated, it can lead to blindness. Moreover, if the new blood vessels disrupt the normal flow of fluid out of the eye, pressure in the eyeball can elevate. This buildup can damage the optic nerve that carries images from the eye to the brain, resulting in neovascular glaucoma – a severe form of secondary glaucoma which is generally associated with poor visual prognosis.
Warning signs and symptoms of diabetic retinopathy
At first, diabetic retinopathy in the early stages might cause no noticeable symptoms, therefore patients are unaware of it and routine eye screening is often omitted. As the condition progresses over time, common manifestations include:
- Spots, dark strings or floaters floating in the vision
- Distorted vision
- Blurred and fluctuating vision
- Color distinguishing problem
- Dark areas in the vision
- Vision loss
**The severity of symptoms is widely varied among individuals. Some patients with advanced stage of diabetic retinopathy might not experience any abnormalities.
Diagnosis of diabetic retinopathy
Patients with diabetes are highly recommended to annually screen for diabetic retinopathy even if they have exhibited no abnormal signs or symptoms. Diabetic retinopathy is diagnosed by a comprehensive dilated eye exam. During this eye exam, eye drops are placed in the eyes to dilate the pupils, allowing the ophthalmologist a better view inside the eyes. The eye drops can cause blurred vision until their pupil dilating effects wear off, taking 4-6 hours. On that account, patients are not advised to drive themselves after having their eyes dilated and caregivers or relatives should accompany the patient after the test. In case that any abnormality is not yet detected, an eye screening test and dilated eye exam should be regularly conducted on a yearly basis. Nevertheless, if diabetic retinopathy has been diagnosed, further investigations and treatments might be required, depending on its stage and severity. Instead of an annual test, more frequent eye exams might be indicated to monitor treatment outcomes and disease progression.
Treatment of diabetic retinopathy
Treatment of diabetic retinopathy is aimed at slowing or stopping the disease progression. Treatment plan for each patient depends primarily on the stage and severity as well as other comorbidities.
- Treatment of early diabetic retinopathy: For mild or moderate nonproliferative diabetic retinopathy, immediate treatments might not be necessarily indicated as well-controlled blood sugar levels including a glycosylated hemoglobin (HbA1c) can substantially slow the disease progression. Moreover, maintaining blood pressure and blood lipids within desired ranges can also help mitigate disease severity. Close and frequent monitoring enables the abnormal signs to be detected at its earliest stages, allowing an accurate diagnosis and effective treatment to delay progression while preventing vision loss.
- Treatment of advanced diabetic retinopathy: If the condition advances, prompt treatments are often required, including:
- Laser treatment: Laser treatment is used to treat the growth of new blood vessels at the back of the eye (retina) in case of proliferative diabetic retinopathy and maculopathy. Treatment can help stabilize the changes in the eyes caused by diabetic retinopathy and prevent vision from getting worse, although it does not usually improve the sight.
- Injecting medications into the eye: Medications, called anti – vascular endothelial growth factor (anti-VEGF) are injected into the vitreous of the eye aiming at prohibiting growth of new blood vessels in the eye, decrease fluid buildup and relieving macular edema. These medications can help prevent the vision from worsening or perhaps improve vision acuity. In some cases, steroidal drugs might be an alternative option.
- Vitrectomy: If severe complications develop, e.g. vitreous hemorrhage, scar tissue tugging on the retina or retinal detachment, macular edema and retinal tear, vitrectomy – a surgery to remove blood from the vitreous humor might be potentially suggested in order to prevent permanent vision loss.
Preventing vision loss caused by diabetic retinopathy
- Keep blood sugar, blood pressure and blood lipids under control
- Refrain from smoking and alcohol drinking
- Pay extra attention to vision changes, especially when vision suddenly becomes unclear, spotty or hazy.
- Schedule a yearly eye exam despite no abnormal sign has yet exhibited.
Although diabetic retinopathy cannot be completely prevented, regular eye exams, good control of blood sugar, blood pressure and blood lipids, as well as early intervention for vision problems can help prevent severe vision loss.











