The kidneys filter wastes and excess fluids from the blood, which are further excreted in the urine. Chronic kidney disease is characterized by the gradual loss of kidney function. When it eventually reaches an advanced stage, dangerous accumulations of excessive fluid, electrolytes and wastes can build up in the body. Chronic kidney disease can slowly progress to end-stage kidney failure, which becomes fatal without hemodialysis (an artificial filtering) or a kidney transplant. Once end-stage kidney develops, the patients need to have dialysis treatments for the whole life unless they are able to get a kidney transplant. A vascular access makes life-saving hemodialysis treatments possible since it substantially reduces the risk of infection while improving the quality of hemodialysis in the long run.
Get to know chronic kidney failure
Chronic kidney disease is described as a lasting damage to the kidneys that can usually get worse over time. Chronic kidney disease leads to an impaired ability of the kidneys to filter and excrete fluids and wastes. If the kidney damage severely progresses, the kidneys may stop working, resulting in “chronic kidney failure” or end-stage renal disease. Signs and symptoms of chronic kidney failure indicating that hemodialysis is required are as follows:
- Swelling of the body and extremities from fluid retention;
- Unhealthy pale skin due to the build-up of wastes or toxins;
- Unexplained shortness of breath or breathing difficulty;
- Decreased urine output and
- Elevated blood pressure.
Vascular access for hemodialysis
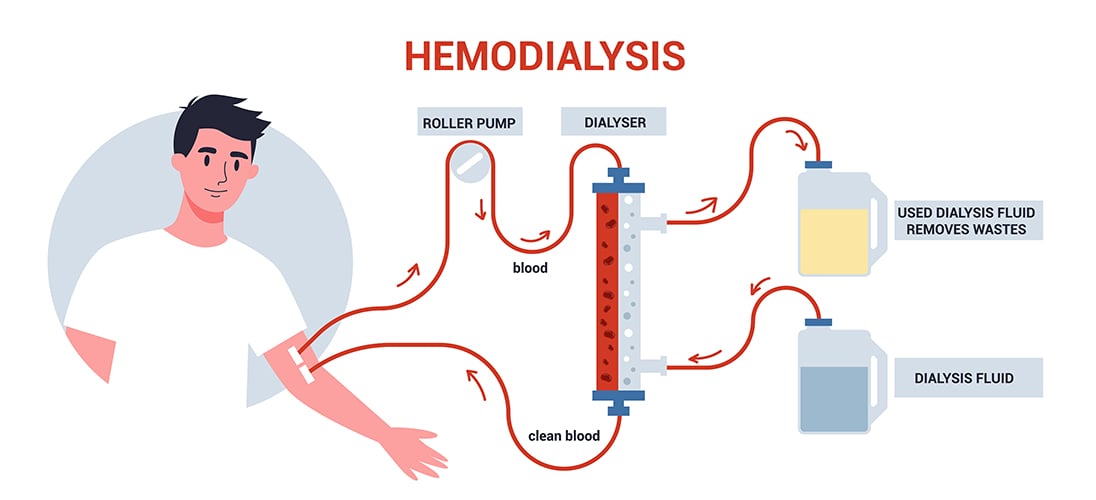
Hemodialysis artificially removes waste products and excess fluids from the blood when the kidneys can no longer perform its function. Hemodialysis uses a machine to filter waste substances by sending the patient’s blood through a filter, called a dialyzer, outside the body. The vascular access is a surgically created vein used to remove and return blood during hemodialysis. The blood goes through a needle and then travels through a tube that takes it to the dialyzer. Inside the dialyzer, the blood flows through thin fibers that filter out waste products and extra fluid. The machine returns the filtered blood to the body through another tube. A vascular access allows for large amounts of continuous blood flow during hemodialysis treatments to filter as much as possible per treatment. Each hemodialysis treatment takes approximately 4-5 hours. Patients with end-stage kidney failure usually undergo hemodialysis 2-3 times per week for their entire lives unless they are able to get a kidney transplant.
Vascular access
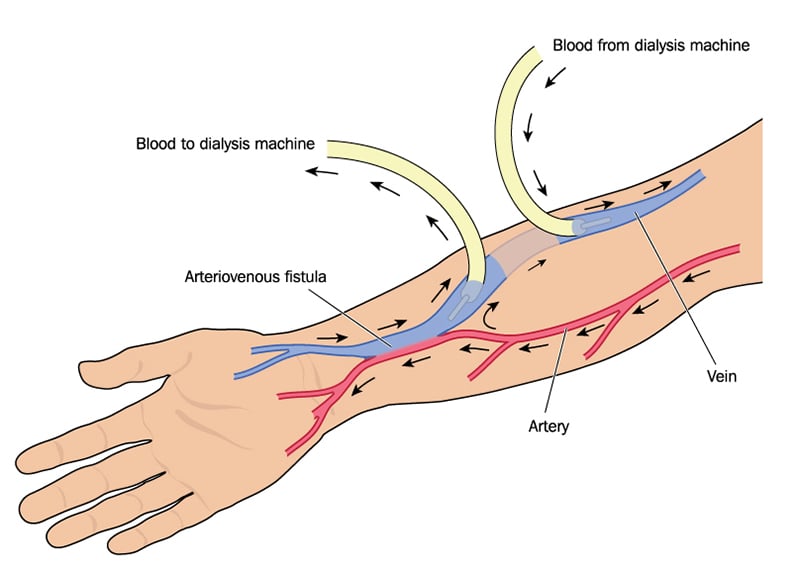
A vascular access, an arteriovenous (AV) fistula is a surgical connection made between an artery and a vein, created by a vascular surgeon. An AV fistula is typically located in the wrist in non-dominant arm. However, if the vessels in the wrist are too small, the vessels in the forearm or upper arm might be used instead. With an AV fistula, blood flows directly from the artery into the vein, resulting in an increased blood pressure and amount of blood flow through the vein. The increased flow and elevated pressure cause the vein to enlarge, allowing for the capability of delivering the amount of blood flow necessary to provide an adequate hemodialysis treatment. An AV fistula is the preferred vascular access for long-term dialysis since it lasts longer than any other dialysis access types and it is less prone to infection and clotting. Before the procedure takes place, local anesthesia will be administered to numb the local area and minimize pain where the vascular surgeon creates the AV fistula. Patients can normally go home afterwards.
Types of vascular access
There are two types of vascular access designed for long-term use: an arteriovenous fistula (AVF) and an arteriovenous graft (AVG). To choose the type of vascular access, it is based upon anatomy and life expectancy as well as personal conditions among other factors.
- An arteriovenous fistula (AVF)
An AVF connects an artery to a vein, aiming at causing extra pressure and increased blood to flow into the vein, making it enlarge and strong which provides easy and reliable access to blood vessels. An AVF frequently requires 4-6 weeks to mature before the first hemodialysis treatment begins. To obtain successful an AVF maturation, preferred veins for fistula creation should meet these criteria:- Having measured diameter larger than 6 mm.
- Being less than 6 mm. deep from skin surface
- Having minimum blood flow rate at least 600 ml/minute
- Being relatively straight
In addition to providing good blood flow for hemodialysis, benefits of an AVF include:
- Lasting 4-5 years which is longer than other types of access
- Possessing lower chance of procedure-related complications, e.g. fewer infection rates and less blood clots
Key components of AVF maturation are adequate dilation of the outflow vein, quality of the vein, strength of the wrist, concentration of the blood and the occlusion of the vessels.
- An arteriovenous graft (AVG)
An AVG is a deliberate connection between an artery and vein that is created by interposing graft material between them. An AVG is primarily considered if the vessels are inapplicable or too small to perform an AVF. The size of the vessels that is suitable for creating an AVG ranges from 2 to 2.5 mm. Similar to an AVF surgery, a looped, plastic tube is placed to connect an artery to a vein. An AVG can be used within a day up to 3 weeks after the surgery, depending the graft materials. Nonetheless, in comparison to an AVF, an AVG is more costly and likely to causes certain problems, e.g. infection and clotting which can block blood flow through the graft. Moreover, it usually lasts shorter compared to an AVF, even though a well-cared-for graft might last several years.
Vascular access procedure
To perform vascular access surgery, the steps are described as follows:
- The access area will be cleaned before surgery begins.
- After local anesthesia administration, a 3-cm. skin incision will be made.
- An artery and a vein will be sewn together, creating a larger, tougher vein that can tolerate multiple needle punctures that are needed for hemodialysis.
- A bruit (a rumbling sound that the patients can hear) or a thrill (a rumbling sensation that the patients can feel) can be subsequently perceived.
- Bleeding will be controlled before an incision closure.
To complete the procedure, an approximate time consumption is 30 minutes up to an hour.
Challenges of vascular access
- Patients are unable to lay flat for an hour
- Arms are excessively large
- Small arteries and veins
- Hardened arteries caused by calcified plagues on the artery walls.
When should vascular access for hemodialysis be considered?
- Vascular access for hemodialysis is considered essential when kidney disease reaches stage 5 which is an end stage, in which GFR (glomerular filtration rate) falls below 15 mL/min/1.73 m2.
- After reaching end stage kidney disease, hemodialysis must be conducted within 6-12 months.
- Emergency hemodialysis might be required if serious complications exhibit, e.g. significant reduction in urine output, lethargy, weakness, metabolic acidosis or the buildup of acid in the blood, edema and electrolyte imbalance.
If vascular access has not been yet prepared, emergency hemodialysis can be conducted by inserting a plastic tube ( catheter) into a large vein in the neck. And it will be used for hemodialysis until an AV fistula becomes completely matured, up to 6 weeks.
Preparations prior to vascular access surgery
- Before AV fistula surgery, physical examination and vessel mapping uses Doppler ultrasound will be performed in order to evaluate blood vessels and overall health status.
- Underlying conditions, such as diabetes and hypertension must be kept under control prior to surgery .
- Blood draw, blood pressure measurement, IV fluid infusion or injection conducted in the selected arm for creating vascular access must be strictly avoided since the vessels can be profoundly affected.
- It is unnecessary to refrain from foods and fluids before procedure begins.
- To strengthen the vessels that will be used for vascular access, it is recommended to do upper extremity exercise by squeezing and relaxing the ball 10-15 minutes, 3 to 4 times each day.
Care after surgery
Patients can care for and protect a vascular access by
- Continuing wound dressing 1-2 times/week, for XXXX Stitches// Dissolvable sutures?? need to be removed 2-3 weeks afterwards.
- Keeping the access clean and dry at all times. Being careful not to bump or cut the access.
- Avoiding wearing tight clothes and jewelry, such as ring and bracelet over the access site. Not sleeping with the access arm under the body and lifting heavy objects or putting pressure on the access arm.
- Avoiding injection, blood draw and putting a blood pressure cuff on the access arm.
- Using the access site only for hemodialysis and using the access arm as usual for reducing swelling which sometimes develops after surgery. Lifting the access arm above the heart while sleeping to minimize swelling. Swollen arm is spontaneously resolved within 2-4 weeks.
- Doing upper extremity exercise by squeezing and relaxing the ball using the access arm to enhance successful maturation while strengthening the vessel walls.
- Checking the thrill in the access site every day. The thrill is the rhythmic pulse vibration that the patients can feel over the vascular access. It is used to indicate the effectiveness of the vascular access. If the thrill is impalpable, an immediate medical assistance must be sought.
- Watching for signs of abnormality and infection, including excessive bleeding, redness, swelling, pain, numbness and tenderness at the access site as well as fever and cold fingers or hand with a pale or blue-purple discoloration. If any of these conditions arise, an medical care is urgency required.
Advantages of vascular access
- Short-term hemodialysis by inserting a venous catheter into a vein in the neck, chest, or leg near the groin can be avoided as it carries certain risk for developing complications, including blood clot, infection of the vein or a scarred vein and fluid buildup in the lung and chest cavity.
- Daily activities can be resumed, such as showering and swimming.
- An emergency dialysis through the neck can be avoided.
Disadvantages of vascular access
- All types of vascular access possess long-term complications, including low blood flow due to blood clotting in the access, hand or arm pain during hemodialysis, swollen arm, access infection and enlarged blood vessel wall (aneurysm) that can potentially lead to rupture, resulting in severe bleeding.
- An AVF might induce or exacerbate heart failure when the blood overflows via the fistula.
- Access infection is found more frequently in an AVG than an AVF.
The success of vascular access for long-term hemodialysis depends chiefly upon several determinant factors, including the characteristics of selected vein and artery, blood concentration, blood clotting and the strength of the wrist and arm. To ensure the best possible outcome in access maturation with a high degree of safety, vascular access must be conducted by highly experienced vascular surgeon in the hospital accredited with international standards.






