An anal fistula is defined as an infected tunnel that develops between the skin and the muscular opening at the end of the anus. In most cases, an anal fistula is the result of infections that begin in an anal gland. If it is left undiagnosed or untreated, infections become chronic, causing frequent anal abscesses. Owning to certain similarities in clinical manifestations, e.g. rectal bleeding and pain during bowel movements, an anal fistula is often mistaken for hemorrhoid, leading to inappropriate treatments. If warning signs and symptoms of an anal fistula exhibit, immediate medical attention must be sought, allowing accurate diagnosis and effective treatments in a timely manner before the condition progresses and complication arises.
Get to know an anal fistula
An anal fistula, as an abnormal passage, is a small tunnel that connects an infected cavity (an abscess) in the anus to an opening on the skin around the anus. Inside the anus, there are a number of small glands that produce mucus, known as anal glands. At times, these glands might get clogged and become infected after exposure to fecal bacteria, leading to a pus-filled abscess that drains spontaneously or surgically through the skin next to the anus. The fistula tract then forms a tunnel under the skin and connects the anal canal to the skin of the buttocks. Up to half of these abscesses may develop into fistulas.
Types of an anal fistula
Regarding severity degrees, anal fistulas can be categorized as simple fistula and complex fistula:
- Simple fistula presenting with a single opening tract connecting the anus to the skin with less involvement of external anal sphincters – a layer of voluntary muscle encircling the outside wall of the anal canal and anal opening.
- Complex fistula mostly presenting with multiple tracts connecting the anus to the skin or surrounding organs. Complex fistula significantly disrupts the external sphincter that may lead to fecal incontinence.
Causes of an anal fistula
The major contributing causes to an anal fistula are clogged anal glands and anal abscesses. Approximately 50% of these abscesses can develop into a fistula, despite abscesses drain spontaneously or are drained surgically. Other conditions that may cause an anal fistula include:
- Crohn’s disease (an inflammatory disease of the intestine)
- Certain sexually transmitted diseases, e.g. syphilis and chlamydia
- Certain infection diseases, e.g. actinomycosis and tuberculosis
- Anal cancer or certain type of skin cancer developing around anus area.
Signs and symptoms of an anal fistula
Manifestations of an anal fistula might widely vary among individual while some might experience intermittent symptoms. Common signs and symptoms of an anal fistula include:
- Pain and swelling around the anus or buttocks.
- Bloody or foul-smelling pus from an opening around the anus.
- Itchy skin or irritation of the skin around the anus from drainage.
- Frequent anal abscesses which usually cause pain with bowel movements.
- Fever, chills and a general feeling of fatigue.
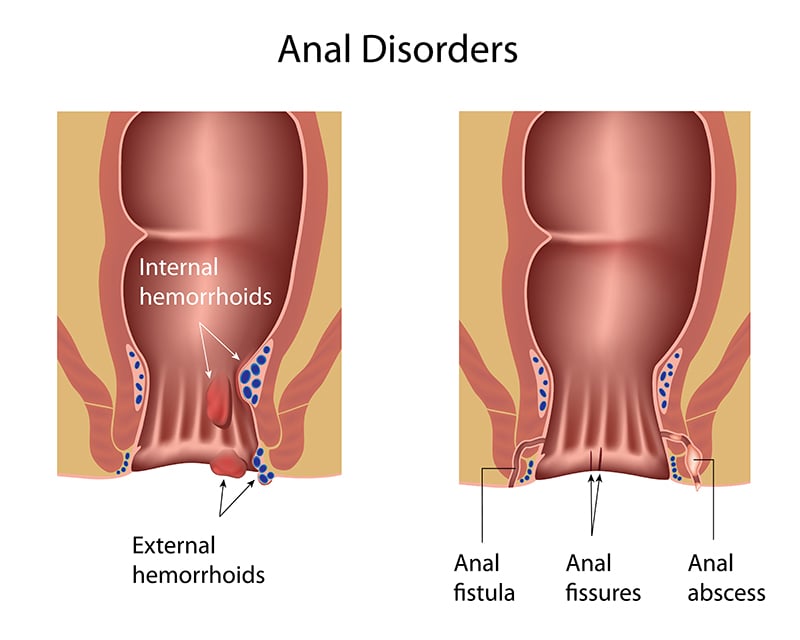
Characteristics of hemorrhoid VS. anal fistula
|
Hemorrhoid |
Anal fistula |
|
Rectal bleeding during bowel movements |
Bloody drainage |
|
No pus |
Foul-smelling pus exhibiting along with fever |
|
Protruding piles (hard lumps) with straining during bowel movements |
No protruding piles |
|
Pain around the anus during bowel movements |
Constant pain around the anus even without bowel movements |
|
High recurrence rates. |
Recurrent rates are considerably low. |
|
Usually self-limiting if not advanced |
Most cases require treatment interventions. |
Diagnosis of an anal fistula
To diagnose an anal fistula, medical history taking and physical examination will be conducted by the colorectal specialist. During physical examination, the specialist thoroughly examines the area around the anus, looking for an opening (of the fistula tract) on the skin. Imaging tests may be used to aid in the diagnosis, such as an endoanal ultrasonography to assess the anatomy of the anal canal using an ultrasound scanner. In case that complex fistulas are detected, a Pelvic MRI (Magnetic Resonance Imaging) is often used to obtain a better visualization of the fistula tracts. If a simple fistula is left untreated, it can potentially progress to a complex fistula.
Treatments of an anal fistula
Treatments of an anal fistula are comprised of these following approaches:
- Anal abscess drainage: Under most circumstances, anal abscess can be surgically drained to remove a pocket of pus that has built up within the anal area. Surgical drainage is often considered along with the administration of antibiotic and anti-pyretic drugs. However, the rates of anal fistula after the drainage are considerably high, up to 50%.
- Anal fistula surgeries: Surgery is an effective option to cure an anal fistula. The goal is a balance between getting rid of the fistula while protecting the anal sphincter – the muscle around the anus, which could cause incontinence if damaged. Due to advances in surgery, several surgical options are available. The most appropriate surgical technique for each patient is determined by the colorectal specialist, hinging upon symptoms and disease severity. Surgical approaches to treat anal fistulas are:
-
- Ligation of Intersphincteric Fistula Tract or LIFT procedure: The LIFT procedure is a relatively new technique involving ligation and division of the fistula tract in the intersphincteric space. Using an intersphincteric approach the tract can be identified and ligated without causing the damages to the muscle. As a promising sphincter-preserving procedure, the LIFT procedure usually brings back quality of life to the patients as continence can be well preserved.
- Fistulotomy: This procedure opens up the fistula tract using surgical knife or electrocautery in a way that allows anal fistula to heal from the inside out. After wound dressing and keeping wound unsealed, wound healing process takes approximately 4-6 weeks. The procedure may be considered for the patient with superficial anal fistula.
- Seton placement: Seton placement procedure in usually recommended for complex fistulas. It involves placing a suture or rubber band (a Seton) in the anal fistula that, in some cases, needs to be progressively tightened. The procedure enables the fistula to heal behind the Seton and reduces the risk of incontinence.
- Fistulectomy: Fistulectomy is a surgical procedure in which all fistula tracts are completely excised. Due to possible sphincter muscle injuries, it might result in fecal incontinence after surgery.
In the case of the fistula which may be complicated by an abscess, adequate drainage is required prior to the definitive anal fistula treatments. Most anal fistulas are treated successfully by surgical interventions. Nevertheless, each fistula treatment procedure may result in different potential outcomes and complications, particularly the recurrence rates and bowel incontinence. Detailed discussion with the colorectal specialist about the success rates and potential risks prior to the treatment is highly recommended.
Prevention of recurrent fistulas
After treatment, the risks of recurrence can be minimized by following the instructions:
- Keep immune system strong.
- Take high-fiber diet.
- Drinking plenty of water or fluid.
- Smoking cessation.
- Regular exercise.
- Avoid constipation by using a stool softener or bulk laxative when needed.
- Keep a good anal hygiene.
- For diabetes, blood sugar should be closely monitored.