Vascular access problems can usually develop in patients who need frequent administration of intravenous fluids or drugs and blood transfusion. Particularly in cancer patients who undergo several cycles of chemotherapy that requires intravenous treatments and blood collections for treatment monitoring, the most common vascular challenges are vascular complications, e.g. vessel hardening, thrombosis, leakage, irritation and inflammation. As a result, these vascular problems substantially lead to vascular access difficulties which largely affect drug administration and treatment efficacy, besides other relevant complications. Medical devices called catheters and ports make intravenous treatments easier. An implanted chemo port is an implanted medical device allowing easy access with convenience to the veins for chemotherapy. The key advantage of this vein-access device is that chemotherapy medications can be directly delivered into the port rather than a vein. This device eliminates the need for needle sticks while avoiding repetitive injuries or damages to the veins. Patients with an implanted chemo port implantation can continue their daily lives and activities without limitations. In addition, an implanted chemo port helps to minimize the risk of vascular complications, allowing for an improved patient’s quality of life with less medical expenditure spent during treatment.
Get to know an implanted chemo port
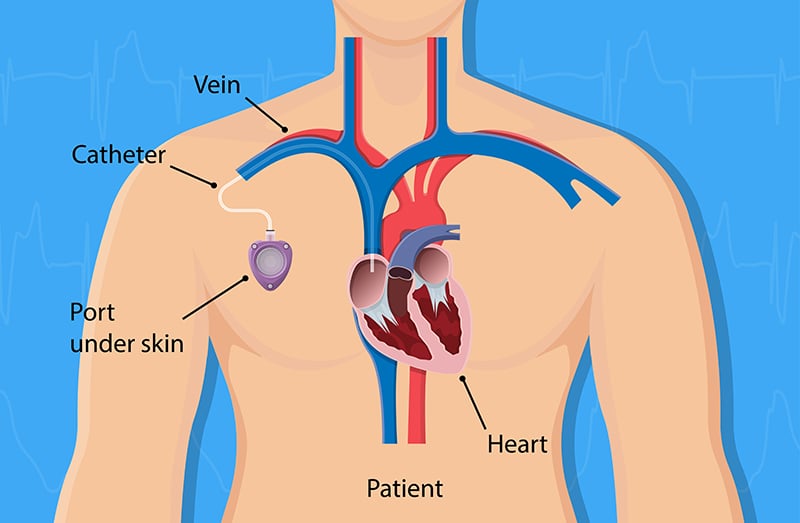
An implanted chemo port is an implantable device that is surgically placed under the skin, usually in the right side of the chest or occasionally in the upper arm. A port is attached to a thin, flexible tube, called a catheter that is threaded into one of the central veins above the right side of the heart (usually the jugular vein, subclavian vein or the superior vena cava). Once a port is placed, an imaging test, X-ray will be used to ensure that the end of the port catheter is in the proper position. A slight protrusion of the skin over the port might be palpable. A port can be used to draw blood and infuse chemotherapy drugs. Moreover, it can also be used for blood transfusions. Without vessel punctures, during blood draws or chemotherapy infusions, a needle can be simply inserted into an area called the septum which is made of a special self-sealing silicone that can be repeatedly punctured thousands of times by a needle before the strength of the material is compromised. Resealable septum contributes to a very low risk of infection.
An implanted chemo port is considered an effective vascular access option for patients who need to undergo long-term intravenous treatments using chemotherapy drugs or certain medicines with high concentration. It is also an option for patients presenting with vascular problems, such as failed attempts to find suitable intravenous lines. Due to medical advances, the latest implantable vascular access port system, PORT-A-Cath®POWER P.A.C comes with the additional option of power injecting contrast media during CT or MRI procedures.
Component of an implanted chemo port
A port is a small, implantable appliance that is surgically placed beneath the skin. It is made of medical grade materials silicone which are biologically compatible with body tissues. An implanted chemo port consists of 3 main components:
- The portal. A small chamber sealed at the top with the septum made of self-sealing silicone that can be punctured repeatedly. Portals are made of titanium, stainless steel or special plastic. The portal capacity is 0.3-0.7 ml.
- The catheter. Catheter is a thin flexible tube used to thread into one of the large veins. It is made of flexible silicone that does not affect or cause any damage to the lining of the inner surface of the veins.
- The catheter connector. This component connects the catheter to the portal. The catheter connectors are usually made of titanium and/or plastic.
Why is an implanted chemo port needed?
An implanted chemo port is indicated for patients requiring frequent and long-term intravenous therapies, such as chemotherapy for cancer patients. Having a port allows healthcare professionals easy access to a major vein with low risk of infection. An implanted chemo port is centrally placed under the skin near a large vein in the upper chest while an intravenous (IV) catheter is peripherally placed in an arm or hand vein. Sometimes, suitable IV site can be difficult to find, causing failed intravenous attempts for drug administration and blood draw. Due to easy and convenient access to the veins, an implanted chemo port provides a safer and more efficient medication delivery process without repetitive vessel punctures that often cause pain and other undesired effects. Especially in cancer patients who need to receive several cycles of chemotherapy, phlebitis –an inflammation of the vein is a serious vascular complication usually caused by chemotherapy drug administration through peripheral veins in the arm or hand. Moreover, certain chemotherapy drugs are vesicant agents, causing severe irritation and damages to the surrounding tissues if there is any leakage from the vein while being administered intravenously. Unlike an IV catheter which needs to be reinserted for each treatment session, an implanted chemo port can remain in place as long as necessary – for several weeks or even years. When it is no longer required, the device can be removed through an outpatient procedure.
Main advantages of an implanted chemo port
- It helps to avoid puncture wounds and damages directly to the veins in the arm or hand. Since the procedure is conducted with a sterile technique, the risk of infection drastically decreases.
- Easy and convenient intravenous access results in less pain and more comfort while improving patient’s quality of life.
- A port can be used for delivering drugs, fluids and transfusions as well as drawing blood for laboratory testing and injecting contrast media for imaging procedures.
- After placement, daily lives and activities can be resumed without restrictions.
- An implanted chemo port helps streamlining the delivery of chemotherapy medications. It also minimizes the risk of medications coming into contact with body tissues and skin.
Placement of an implanted chemo port
The implantation of a port is considered a minor procedure performed under local or general anesthesia by an interventional radiologist or vascular surgeon. The port is usually placed under the skin and inserted in the upper chest (known as a chest port), just below the clavicle (collar bone) or occasionally in the upper arm (known as an arm port). With one or two small incisions (sized 1-2 inches), the catheter is threaded into one of the large veins (usually the jugular vein, subclavian vein or the superior vena cava) and attached to the portal chamber. Once placed, an x-ray is then used for post-operative imaging to confirm appropriate placement position of the port. After placement, the skin around the port remains unchanged. However, a slight protrusion of the skin over the port enables the implanted port to be accessed easily. After the procedure, fluids and medications can be instantly administered as prescribed.
How to use an implanted chemo port
To access the implanted port, a special non-coring needle will be inserted through the skin and the portal septum. Since the needle goes through the skin, the patients might feel a pricking sensation. To mitigate pain during needle puncture, a local anesthetic drug needs to be applied to temporarily numb the skin 30-45 minutes before accessing the port. However, this discomfort sensation may subside over time. The medications or fluids can flow through the needle into the portal chamber and through the catheter directly into the central veins and the blood circulation. The medications or fluids are given into the system by using a syringe as IV push or as a continuous infusion through medication bags without an infusion pump. Before removing the needle, flushing with low-dose heparin as an anticoagulant is essential in order to prevent clot formation as well as port and catheter occlusion.
Instructions prior to port placement
- Concerning medical clearance before performing a procedure, relevant tests, e.g. blood test, electrocardiography (EKG) and chest X-ray need to be completed, depending on physician’s considerations and patient’s conditions which might vary from person to person.
- Adequate rest should be obtained before surgery. It is recommended to refrain from eating and drinking at least 6-8 hours before surgery begins. All medical advices must be strictly followed.
- If the patients are taking any medicines that thin the blood, such as antiplatelet and anticoagulant medicines, the physician should be informed as these medications might need to be temporarily discontinued before surgery.
- In case any question or concern regarding the procedure, please ask more information from the physician.
Instructions after port placement
During the first week, these instructions should be followed:
- During the first 24-48 hours, patients may have some discomfort at the incision sites, such as swelling, bruise and pain. If pain develops, pain-relievers can be taken as prescribed. Pain should subside within 48 hours after surgery.
- After procedure, patients can take a shower as usual since the incision sites will be tightly covered by waterproof bandages with adhesive seals for 5-7 days. Keep the dressing dry every time after showering.
- Vigorous exercise or activities are not advised. Lifting anything heavier than 1 kilogram must be also avoided since it potentially aggravates pain and inflammation.
- It is generally best to sleep on the back to prevent any friction or movement to the port. If the patients need to sleep in any position other than flat on their back, it is advised to sleep on non-port side.
- Follow-up appointment will be made a week after surgery.
Possible complications
Infection is the most common complication of venous port system use among cancer patients who receive long-term chemotherapy. If infection develops, it can potentially lead to catheter-related blood stream infections (catheter-related sepsis). If a special non-coring needle is not properly inserted through the portal septum, leakage of chemotherapy drug during administrating can cause tissue and vascular damages under the skin around the port area.
Immediate medical attention must be sought if any of these signs and symptoms arise:
- Bleeding at incision sites
- Progressive swelling and redness at incision sites
- Severe pain at the incision sites accompanied by shoulder pain and inability to lift the arm on port side.
- Swelling arm on port side
- Chest discomfort, chest tightness or difficulty breathing
- Wound pus or wound drainage
- Fever (core body temperature greater than 38.5’c) or chills
Caring for an implanted chemo port
- After removing the needle from the portal, transparent waterproof bandage must be used to tightly seal the puncture site for 24 hours. If allergic reaction develops after applying the bandage, please keep medical staff informed immediately.
- Do not scratch the puncture site. If the skin over the port turns to be red or inflamed, immediate medical attention is needed.
- If the skin over the port has any open wound, refrain from water and keep it dry.
- If the portal or needle seems to have moved or abnormal symptoms arise, e.g. fever, pain, swelling or redness over the port area, inability to lift the arm on port side, chest discomfort, breathing problems and drainage or bleeding at the incision sites, please seek medical attention immediately.
Recommendations
- All medical advices must be strictly followed. For instance, the implanted port must be regularly flushed with a heparin solution every 4-6 weeks to prevent clot formation and catheter occlusion while maintaining access or to discontinue access.
- To access the port, only a special non-coring needle is allowed to use.
- If any abnormal sign or symptom exhibits, such as fever, chills, pain or swelling at the incision site, medical attention is needed immediately.
- Once the port is implanted, a given wallet-sized identification card must be kept with the patient at all times while receiving treatments.
- Do not skip any medical appointment.
How long can an implanted chemo port remain in place?
On average, the portal septum made of a special self-sealing silicon can be repeatedly punctured 1,000 -2,000 times by using a special needle before the strength of the material is compromised. Unlike an IV catheter, which needs to be reinserted for each treatment session, an implanted chemo port can remain in place as long as necessary – for several weeks or even years. When it is no longer needed, the device can be removed through a outpatient basis procedure. To remove the port, local or general anesthetic is used to numb the area of the incision over the port. A small incision will be made over the port. The port is freed from any tissue and the entire device is removed at once. The skin will be sutured and covered with sterile bandage.
Although an implanted chemo port poses superior advantages over other IV access routes, it carries some catheter-related risks. The most common complication is infection at the port or surrounding area, however, it rarely happens. If abnormal signs or symptoms arise, e.g. swelling or redness over the port site, fever, chills and breathing difficulties, immediate medical assistance must be obtained. In addition, several types of catheter occlusion can occasionally develop as noninfectious complication. Depending on occlusive degree, the line can be flushed using heparinized solution, an anticoagulant to unclog the clot or occlusion. In case of complete occlusion, the device needs to be surgically removed. To ensure the best surgical outcome with safety, port placement should be conducted by well-trained and highly experienced surgeons in the hospital adhering to international standards.