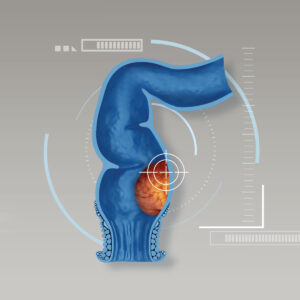
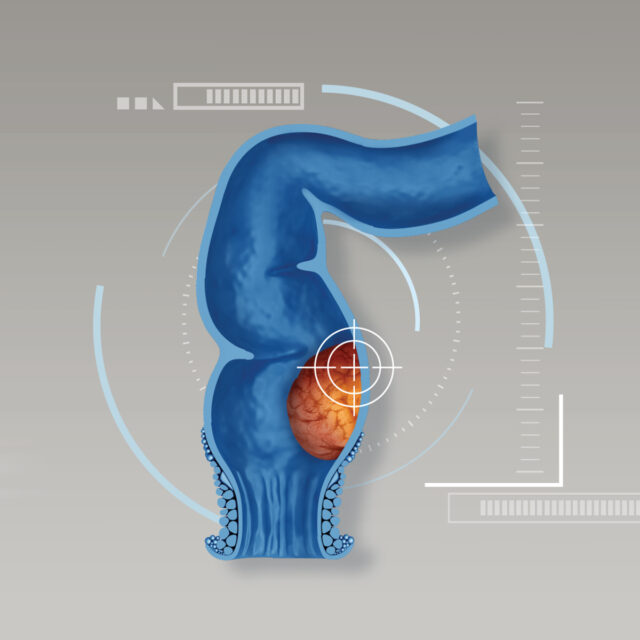
Hemorrhoids are swollen veins in the lower rectum and anus. The veins around the anus stretch due to increased pressure in the lower rectum e.g. pregnancy, being overweight or straining during bowel movements. It eventually leads bulging or enlarged vessels in the anus. Hemorrhoids might develop in different locations at the same time. Classified by locations, there are 2 types of hemorrhoids:
- Internal hemorrhoids: Internal hemorrhoids lie inside the rectum and are covered with cells that line the rest of the intestines. They are deep inside the rectum and not visible from outside. Without complications, they do not usually produce rectal pain, discomfort or irritation in the anal region. However, the hemorrhoids might protrude through the rectum from strain during bowel movement.
- External hemorrhoids: External hemorrhoids are hemorrhoids that affect veins outside the anus. External bulges can be visibly seen and touched around the anal area. They are covered with cells that resemble skin, typically slightly less pink than the surrounding skin. Due to the irritation of surrounding nerve, symptoms might include pain or discomfort, itching or swelling around the anus and rectal bleeding that might be found during defecation.
Possible causes
- Genetic factor: The FOXC2 gene of chromosome 16 might play a critical role in the formation of vessel abnormalities e.g. varicose veins or hemorrhoids.
- Certain occupations that result in increased pressure in the lower rectum. As pressure increases, blood pools in veins and causes them to swell. Eventually, the swollen or enlarged veins stretch the surrounding tissue and hemorrhoids develop.
- Complications of other health-related conditions such as cirrhosis (a late stage of scarring or fibrosis of the liver) and hepatitis B infection with ascites (abnormal buildup of fluid in the abdomen) which causes reduced blood flow to the abdomen.
Signs and symptoms
Hemorrhoids might exhibit different signs and symptoms in different stages:
- Grade I: The internal hemorrhoid bulges into the canal but does not prolapse. These may cause rectal bleeding, especially if accompanied if chronic constipation.
- Grade II: The hemorrhoid protrudes through the rectum with straining during a bowel movement. But it spontaneously returns to the original position once the straining has subsided after bowel movements.
- Grade III: The hemorrhoid protrudes without any straining, especially during exertion that increases abdominal pressure e.g. sneezing, coughing, lifting heavy objects. Protruding hemorrhoids require the patient to push them inside manually.
- Grade IV: The hemorrhoid gets bigger and protrudes through the rectum without straining. Prolapsing hemorrhoid cannot be pushed back. Aggravating symptoms are itchy, swelling or inflamed anus, persistent rectal bleeding and pus or mucus discharge mixed with stool, causing discomfort and severe rectal pain. If left untreated, hemorrhoids are more likely to become infected with severe bleeding which is a major cause for developing anemia, fatigue, fainting and unintentional weight loss.
Diagnosis of hemorrhoids
The majority of hemorrhoid cases have presented “rectal bleeding” which is red bright blood that can be noticed on the toilet paper. More often, patients manifest blood in stool. Presence of swelling, pain or discomfort in the anal region might be possible. If the hemorrhoids protrude through the rectum, patients might develop severe rectal pain that largely interrupts their activities especially when standing up or sitting down. In case of severe bleeding, patients tend to have anemia and become fatigue.
Treatment of hemorrhoids
- Constipation must be avoided. Lifestyle advices include drinking plenty of water and eating high-fiber foods e.g. fruits, vegetables and whole grains. These help to soften the stool and increase its bulk, avoiding the straining that can cause hemorrhoids. If constipation presents, laxative drugs could be considered e.g. magnesium sulfate, emulsion of liquid paraffin (ELP) and bulk-forming laxatives.
- If pain moderately develops due to inflammation, pain killers are needed. Sitz bath (sitting in water up to the hips) is highly advised 2-3 times a day, 15-30 minutes each time. Generally, rectal suppositories are prescribed to alleviate symptoms for 7-10 days.
- In case that anemia develops from bleeding, iron supplements are given additionally.
- If hemorrhoids externally protrude through the rectum, patients should wear gloves and use the finger trips soaked with soap to push prolapsing hemorrhoids back into the rectum. If unsolved, medical attention must be sought as soon as possible.
- If rectal bleeding persists longer than 1 week or regularly comes and goes with the presence of other suspected conditions especially in patients aged over 40, colonoscopy is highly advised in order to further investigate colorectal cancer.
- In moderate or severe cases, additional treatments include:
- Injection (sclerotherapy). A chemical solution is injected into the hemorrhoid tissue in order to shrink it by damaging blood vessels and reducing the blood supply to the hemorrhoids. Recommended regimen is a weekly injection for 3-5 weeks consecutively. The success rates of being cured is approximately 60%.
- Rubber band ligation. During this procedure, one or two tiny rubber bands are placed around the base of an internal hemorrhoid to cut off its circulation. The hemorrhoid withers and falls off within a week.
- Hemorrhoid laser procedure. It is a new laser procedure for treatment of hemorrhoids in which hemorrhoidal blood flow feeding the hemorrhoidal plexus is stopped by laser coagulation.
- Surgery (hemorrhoidectomy): Open surgery and minimally invasive surgery.
Preparation before surgery
- Patients are prepared for shaving the surgical areas such as lower abdomen, pubis and anal region. To internally clean digestive tract, bowel irrigation will be done a night before surgery.
- Patients should take a shower, wash hair and trim their nails a night before surgery.
- Patients are instructed not to eat and drink after midnight of the night before surgery.
- Patients should have sufficient rest the night before surgery. Sleeping pills and anti-anxiety drugs might be prescribed.
- During the surgery, patients do not feel pain due to anesthetic drug is injected via spinal cord (spinal anesthesia).
Post-operative instruction
- After surgery, numbness might present in the buttocks, hips and legs due to the lasting effect of anesthetic drugs.
- For proper sleeping position, patients should sleep on either left or right side in order to reduce the pressure that might be placed on the surgical wound. In case that patients underwent spinal anesthesia, to prevent complications that might cause by anesthesia, sleeping on the back is recommended for at least 12 hours.
- After surgery, patients can have regular foods without specific suggestions.
- Sitz bath usually begins on the day after surgery. Sitz bath is a bath in which a patient sits in warm water up to the hips, allowing warm water to heal surgical wound properly.
- If back pain develops after surgery, it must be quickly informed to the doctors or nurse.
Reference: Bangkok Health Research Center