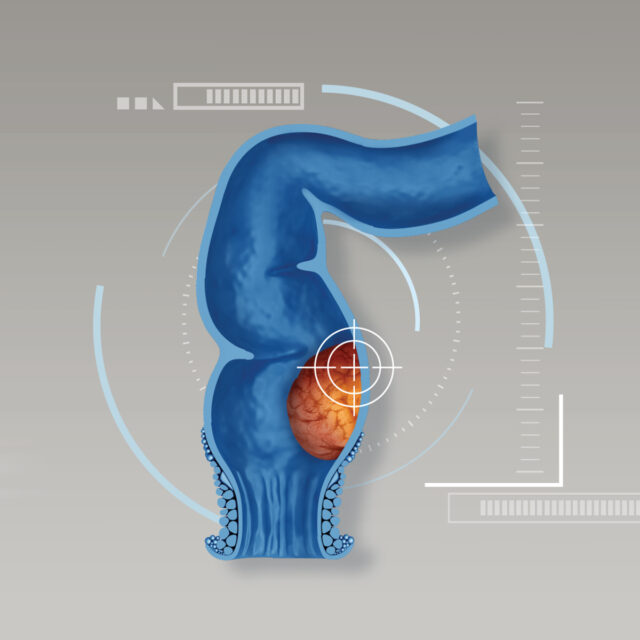
An inguinal hernia occurs when fatty or intestinal tissues protrude through a weak spot in the abdominal muscles. It can appear as a swelling or lump in the groin or as an enlarged scrotum in some men. When inguinal hernias develop, certain concerns are often raised on sexual desires and functions as well as fertility. Regarding clinical studies, certain surgical approach to treat inguinal hernias might disrupt male’s sexual performance. Hence, it is crucial to clarify these issues prior to treatments, allowing relief and better understanding.
Interesting findings derived from the mounting clinical studies related to hernias and treatments are listed as follows:
Men and inguinal hernias
The groin is the junctional area between the abdomen and the thigh on the pubic bone. In the groin area, there are a lot of nerves and vessels that pass within the structure of the inguinal canal supplying the blood to the penis and testicles. In some male patients after undergoing hernia repair with a synthetic mesh implant to reinforce the weakened areas, postoperative complications might possibly develop as synthetic mesh can induce foreign body reactions and fibrosis which sometimes damage the surrounding nerves. As a result, it might interfere with sexual desire and activity. Nevertheless, more clinical evidences are needed in order to draw a definite conclusion.
Inguinal hernias and sexual functions
Ascertained by some clinical studies, most of the patients with uncomplicated groin hernias usually experience a statistically significant improvement of the sexual drive score, erectile function and overall satisfaction within 3-6 months following laparoscopic inguinal hernia repair. Nevertheless, sexual function improvement is similar in patients undergoing both trans-abdominal pre-peritoneal (TAPP) repair and totally extra-peritoneal (TEP) repair. In addition, lightweight and traditional heavyweight meshes appear to yield similar outcomes in terms of sexual satisfaction and sexual function improvement.
Hernia repair and pain affecting sexual function
There are two general types of hernia surgeries: open hernia repair and minimally invasive (laparoscopic) hernia repair. Due to smaller incisions and less invasive to surrounding nerves and tissues, a laparoscopic hernia repair is theoretically thought to result in less pain and faster recovery time. Nonetheless, some clinical evidence has contrarily pointed out that patients undergoing minimally invasive surgery (7.8%) slightly had higher rates of sexual dysfunction than those undergoing open procedures without significance.
Sexual activity after hernia repair
Before and after hernia repair, sexually related pain is primarily located in the groin area and the scrotum. Overall, before surgery, 23 – 32 % of patients complaining about pain during sexual activity. Interestingly, sexually related pain has not increased after hernia repair. Instead, a trend toward a reduction has been reported in some study as only 9-16 % of patients experiencing pain during sexual activity. In the majority of cases, patients can fully recover from pain during sex after surgery within a few months, especially if they have no postoperative complications. Some study reveals that sexually related pain is alleviated by 82% after patients undergoing minimally invasive surgery. However, pain during sexual activity usually presents in 2.3 – 9% of the patients after surgery, regardless of the type of hernia repair.
Inguinal hernias and male’s fertility
Incarcerated hernias as a serious complication of inguinal hernia may cut off the blood supply to one or both testicles which could interfere with sperm production, resulting in less sperm count. In some cases, the vas deferens – a long, muscular tube that transports mature sperm to the urethra in preparation for ejaculation may be damaged by the hernia itself or by the surgical procedure, affecting the flow of sperm during ejaculation. This problem can bring about difficulty for men to conceive through sexual intercourse, even if they are in otherwise perfect health.
Inguinal hernias and the size of testicle
Inguinal hernias do not alter the size of testicle. In fact, inguinal hernias may impair blood supply to some part of the affected testicle (compared to normal testicle). After hernia repair, the blood vessels can be revascularized, allowing the restoration of blood perfusion to the testicles and scrotum. Moreover, both open hernia repair and minimally hernia repair do not induce blood supply disruption and sperm alternation, thus they are not associated with male’s infertility.