People with advanced age are at greater risk of developing a wide range of age-related eye problems, including cataract which is defined as a clouding of the normally clear lens of the eye. Warning signs and symptoms of cataracts usually include clouded, blurred or dim vision, sensitivity to light and glare, seeing halos around lights or distorted colors and need for brighter light for reading or other activities. At first, the cloudiness in vision caused by a cataract may partially affect a small part of the eye’s lens and patients may be unaware of any vision change.
As the cataract grows larger, it clouds more of the lens and distorts the light passing through the lens, causing noticeable symptoms. In spite of fact that there are no studies have yet proved how to prevent cataracts or slow the disease progression, regular eye examinations can help detect cataracts and other eye problems at their earliest stages. If cataract is found, timely and appropriate treatments can be given accordingly, resulting in reduced chances of vision loss and improved quality of life.
Eye evaluation before cataract surgery
- To diagnose a cataract, an ophthalmologist will review symptoms and perform a comprehensive eye examination with several eye tests. If cataract is found, cataract surgery with intraocular lens implants might be indicated. An intraocular lens (or IOL) is a tiny, artificial lens for the eye that replaces the eye’s natural lens and helps clear up the vision after cataract surgery. To customize IOL, before dilating the pupils, a keratometer (or an ophthalmometer) is used to measure the curvature of the anterior surface of the cornea while optical or ultrasound biometry is also used to measure the length of patient’s eyeball.
- After pupil dilation, optical coherence tomography (OCT), a non–invasive imaging test will be conducted in order to determine retinal thickness and investigate each of the retina’s distinctive layers. The measurements obtained by the keratometer are entered into a computer that calculates the correct power for IOL for individuals. Patients will be clearly informed about their lenses and conditions.
- Medical history will be thoroughly taken by an ophthalmologist and nurses. This medical information includes underlying diseases, regular medicines and supplements. Certain medications that affect blood coagulation process e.g. anticoagulant drugs should be discontinued while other medicines for underlying diseases can be taken regularly.
- In case that antiplatelet drugs have been used, an ophthalmologist needs to further discuss with an internal medicine physician whether antiplatelet drugs are allowed to be discontinued 5–7 days before surgery. However, decision making depends on types of medications e.g. aspirin, clopidogrel, cilostazol, warfarin and heparin.
Cataract surgery
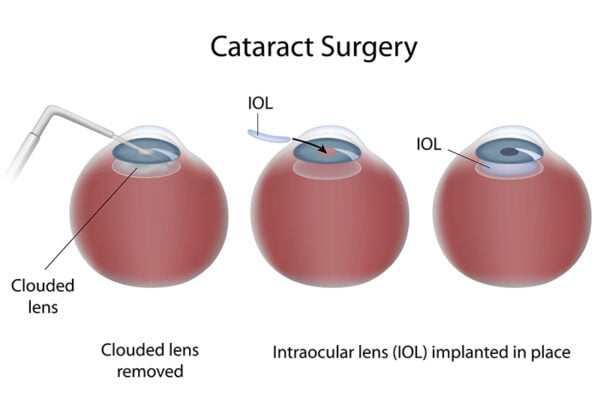
When prescription glasses do not improve vision, an effective treatment for cataract is surgery. Cataract surgery involves removing the clouded lens and replacing it with a clear artificial lens. There are 2 main types of cataract surgery which are:
- Phacoemulsification With Intraocular Lens (IOL) Implantation
Phacoemulsification is a modern cataract surgery method in which the eye’s internal lens is emulsified with an ultrasonic handpiece and aspirated from the eye. This procedure has been widely accepted since it is generally performed on an outpatient basis and only a local anesthetic (either eye drops or injection) is used to numb the area around the eye. It normally takes 30 minutes to complete the procedure. Surgical process involves:
-
- An ophthalmologist makes an incision about 2.4 – 3 mm. on the side of the anesthetized cornea. Then a microscopic circular incision is made in the membrane that surrounds the cataract. An ophthalmologist inserts a small titanium needle (or phaco tip) into the cornea and the ultrasound waves from the phaco tip emulsify the cataract, thus it can be removed by suction. While the cataract is being emulsified, the machine simultaneously aspirates the cataract through a small hole in the tip of the phaco probe. The cortex of the lens can be removed while preserving the posterior capsule, which is used to support IOL.
- After cataract is removed, the foldable IOL is then inserted by an injector into the capsular bag. Since IOL is folded, a larger incision is not required. IOL is selected based on patient’s needs and conditions, such as monofocal lense and multifocal lens. If the patients have astigmatism when the cornea is irregularly shaped or an irregular curvature of the cornea, toric intraocular lenses will be the procedure of choice to correct corneal astigmatism.
- Small incision results in faster wound recovery. No sutures are usually required after the surgery in most cases.
- A day after surgery, patient’s vision will significantly improve and daily activities can be resumed.
- During recovery time, patients are advised to wear an eye shield while sleeping, avoid getting any soap or water in the eyes and refrain from rubbing the eyes (2–4 weeks). Gentle eye cleaning should be strictly applied while taking prescribed medicines both oral drugs and eye drops regularly. All instructions recommended by an ophthalmologist need to be followed.
- Extracapsular Cataract Extraction With Intraocular Lens (IOL) Implantation
An extremely dense cataract requires longer phaco times and higher energy level which carries a higher subsequent risk of corneal decompensation. Similar to phacoemulsification, the purpose of extracapsular cataract extraction is to restore clear vision by removing a clouded or discolored lens and replacing it with an IOL. Extracapsular cataract extraction is older method of cataract surgery that can be used if the cataract is too large to remove with a small incision or too dense (rock-hard) to remove by laser.- An ophthalmologist makes a large incision, 10-mm long, in the eye beneath the iris between the cornea and the sclera wall. The diseased lens is pulled out. The front portion of the capsule is removed and the back part of the capsule remains. IOL is then placed through the incision. Sutures are used to close the incision as the final step.
- Normally IOL used in extracapsular cataract extraction is monofocal lens with a fixed focus for one distance aiming to improve a far vision. Its lifespan is thought to be over a person’s lifetime. Overall results, 95% of patients who undergo this procedure have a better vision after surgery.
Types of IOL
Advances in technology have led to the development of numerous types of intraocular lenses, suitable for the different needs among patients with different conditions. IOL implantation after cataract removal is a foldable lens which can be implanted through small incision on the cornea after the cataract lens is removed. There are several types of IOL. The main types that have been widely used are monofocal lens and multifocal lens. These certain lenses are also used to correct corneal astigmatism.
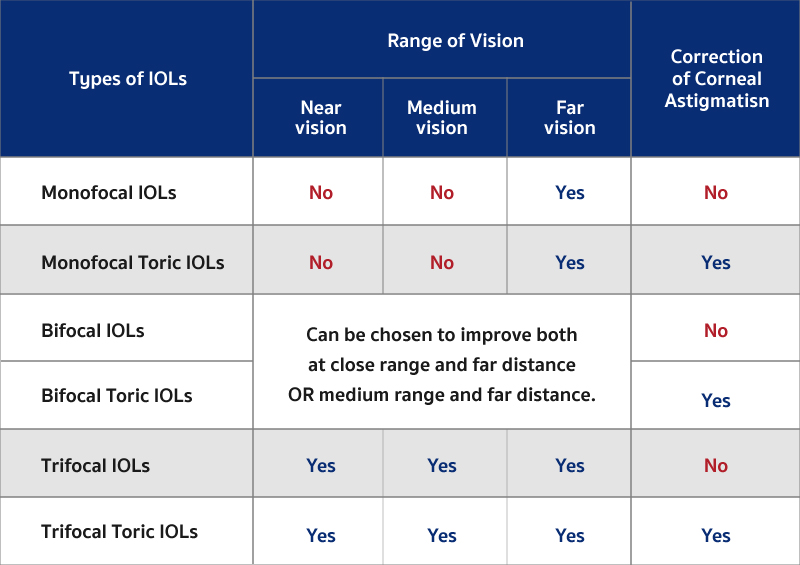
Intraocular lenses for patients without corneal astigmatism
- Monofocal IOLs: They have the same refractive power throughout all the regions of the eye, therefore they are in sharpest focus at only one distance which is a far vision. Patients who have had monofocal intraocular lenses implanted usually require reading glasses.
- Multifocal IOLs: These lenses aim to satisfy focal demands of a wider range of distances (long, medium and short). These lenses allow patients to use less glasses for looking at different distance.
- Multifocal IOLs: These lenses aim to satisfy focal demands of a wider range of distances (long, medium and short). These lenses allow patients to use less glasses for looking at different distance.
- Trifocal IOLs: These lenses aim at increasing the range of vision covering long, medium and short distances without compromising vision quality and less dependent on glasses use.
Intraocular lenses for patients with corneal astigmatism
If cataract is present with corneal astigmatism, toric IOL is often recommended to enhance rotational stability and provide precise visual outcomes with minimal higher order aberrations. Toric IOL has special markers on the peripheral parts of the lens that enable the surgeon to see the orientation of the astigmatism correction in the lens. Types of toric IOL characterized by refractive power include
- Monofocal Toric IOLs: These lenses are able to correct corneal astigmatism. With the same refractive power throughout all the regions, therefore they are in sharpest focus at only far distance. Patients usually require reading glasses for closer vision.
- Multifocal Toric IOLs
- Bifocal Toric IOLs and EDOF Toric lenses: These lenses are able to correct corneal astigmatism while improving focusing on objects both at close range and far distance or medium range and far distance.
- Trifocal Toric IOLs: These lenses aim at correcting corneal astigmatism and increasing all ranges of vision covering short, medium and long distances without dependence on glasses use after surgery
Preparation for cataract surgery
Cataract surgery is done mainly on an outpatient basis, thus most of patients can return home after surgery. However, patient’s vision will be blurred temporarily after surgery, caregivers are needed to take the patient home. Preoperative instructions include:
- Wearing comfortable and loose–fitting clothes.
- Face and hair must be washed before arrival in the hospital.
- Before surgery begins, anesthetic eye drops, dilating eye drops and antibiotic eye drops will be given. For keeping both eyes comfortable during surgery, anesthetic medication can be administered as eye drops or eye injection. However, if patients do not prefer to stay awake, general anesthesia may be considered.
- Cataract surgery usually takes 15-30 minutes. The procedure is conducted in standard operating room. Patients are normally awake for the surgery, but are kept in a relaxed and painless state. While operating, patients might see moving light beams or feel eye compression without pain.
- After surgery is completed, patients need to be closely observed in the recovery room for 30 minutes before returning home. Prescribed oral medications must be strictly taken as instructed. Eye shields must be placed to protect the eyes and eye drops should not be used immediately after surgery.

Postoperative care
- Eyeglasses should be regularly worn to prevent unintentional eye rubbing and eye trauma from accidental rubbing or bumping.
- Patients are advised to wear an eye protective shield on the affected eye while sleeping every night and refrain from rubbing the eye for at least 2 weeks.
- All activities that cause eye trauma, rubbing and bumping must be avoided.
- Eyes must be strictly kept away from water at least 2 weeks or as recommended by an ophthalmologist.
- Instead of facial wash, eyes must be cleaned gently with normal saline and eye cleansing cotton pads to prevent postoperative infections in the eyes.
- To ensure that the eyes will not be moistened by the water, patients should not wash their hair by themselves. It is highly recommended to lie on the back and get hair washed by someone else. While washing, eyes must remain closed at all times.
- All instructions for eye cleaning must be strictly followed.
- Typical follow-up visits occur 1 day, 1 week, 1 month, 3 months and 6 months after surgery. After the first year of surgery, an annual eye check-up is required.
- Lifting heavy objects must be avoided.
- If possible, coughing, sneezing and excessive strain from constipation should be also avoided.
Possible complications
- Although eye infection after surgery is rare because of newer surgery techniques and antibiotic, it is potential complication. Proper eye cleaning and using of prescribed eye drops significantly reduce risks of eye infection.
- Macular cystoid edema may arise 1-2 weeks after the surgery. Macula is the central region of the retina. Macular cystoid edema is caused by retinal swelling or edema, resulting in decreased or distorted vision which is reversible and treatable condition.
- It is possible that a secondary cataract may develop in the remaining back portion of the capsule. This can typically occur several years after the first surgery and impaired vision might gradually occur. However, YAG capsulotomy by using a laser is most often used for the secondary cataract. This outpatient procedure requires no incision. The laser makes a small opening in the clouded capsule to provide a clear path through which the light can pass. As a result, a better vision can be quickly achieved without pain.











