Chronic venous insufficiency (CVI) refers to a condition when the venous wall and/or valves in the lower extremities do not work properly, making it more difficult for blood to return to the heart from the legs. CVI is caused by damaged or weakened valves and vein wall due to aging and prolonged sitting or standing as well as reduced mobility. As a result, blood can flow backwards and pool or collect in these veins, leading to swelling in the lower legs and ankles.
As the condition initially develops, early symptoms include swelling in the lower legs and ankles, followed by aching or tiredness in the legs. These symptoms intermittently present from time to time. If it is left undiagnosed or untreated, more severe manifestations are leathery-looking skin on the legs, flaking or itching skin on the legs or feet and chronic venous ulcers.
The most common causative factors of CVI are blood clots in a deep vein, often in the calf or thigh (known as deep vein thrombosis), swelling and inflammation of superficial vein (phlebitis) and damage or weakening of vein walls due to an advancing age. Besides advancement in age, other contributing factors to the weakened vein walls include diabetes, chronic kidney disease, hypertension, cardiovascular diseases and family history of venous diseases. Owning to the fact that early stage of CVI typically shows non-specific symptoms such as calf pain, it is sometimes mistaken for myositis – an inflammation of muscle. This can impede an accurate diagnosis, resulting in late treatment which potentially brings about advanced CVI presenting with chronic venous ulcers.
Function of the veins
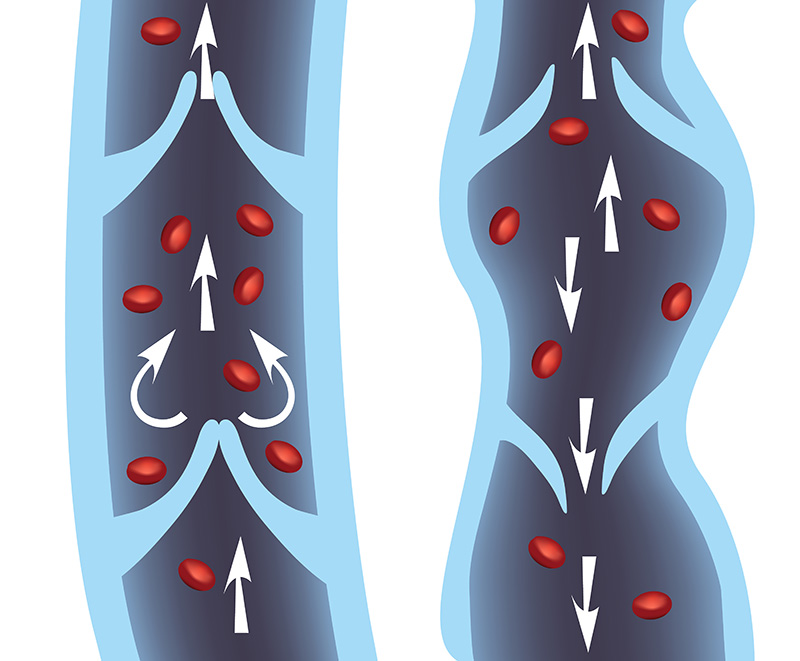
Veins are responsible to return blood to the heart from all the body’s organs, especially in the lower extremities. To reach the heart, the blood needs to flow upward from the veins in the legs and feet. To do so, the relevant muscles regularly contract to squeeze the veins and push the blood upward. Keeping the blood flowing up to the heart and not back down to the legs, the veins contain one-way valves. The veins act as a reservoir, holding 2/3 amount of blood in the body.
The veins are arranged in three systems:
- Superficial Venous System: A superficial vein is a small vein that is close to the surface of the body. It is a small vein comprised of thick lining and valves. The superficial venous system collects blood from the skin and upper layers of tissue in the arms and legs and redirect the blood to the heart.
- Deep Venous System: Contrasting with a superficial vein, a deep vein is a vein that is deep within body, located in the muscles and internal organs. It is a large vein with thinner lining.
- Perforating Venous System or Communicating Veins: Communicating veins are veins that directly communicate the superficial venous system with the deep venous system.
Get to know chronic venous insufficiency (CVI)
CVI is a venous condition in which the venous wall and/or valves in the lower extremities do not function properly, impeding the blood to return to the heart. It is considered one of the most common venous diseases, which include:
- Varicose veins – the swollen and enlarged veins
- Deep vein thrombosis (DVT) – blood clots in veins
- Chronic venous insufficiency (CVI)
Causes of CVI
CVI can be often caused by venous obstruction defined as a partial or complete occlusion of the lumen of a vein that leads to decreased venous flow and venous valvular incompetence. CVI most commonly occurs as the result of deep vein thrombosis (DVT) characterized by a blood clot in the deep veins of the legs. Blood clot and occlusion substantially trigger venous inflammation. Progressing inflammation eventually damages venous valves and venous lining, leading to advanced CVI. If CVI is not treated in a timely manner, the veins can leak or burst, causing the blood accumulation in the surrounding tissues. When this happens, the overlying skin usually presents with a dark brown color. It becomes very sensitive to being broken if bumped or scratched, causing chronic ulcers, especially around the ankles.
Risk factors of CVI
- Family history of venous diseases
- Patients with chronic underlying conditions, e.g. diabetes, chronic kidney disease and cardiovascular diseases.
Grading of CVI
CVI can be classified into 7 grades, based upon clinical manifestations and disease severity.
- Grade 0: Leg or foot pain or heavy leg, leg numbness or warmth, leg swelling and leg cramping at night.
- Grade 1: Reticular veins or spider veins which are enlarged or twisted vessels and visible through the skin.
- Grade 2: Varicose veins with enlarged, swollen or twisted veins.
- Grade 3: Swelling in the legs and feet with uneven size.
- Grade 4: Changes in skin and subcutaneous tissues, e.g. skin discoloration and skin thickening, especially in the foot, around the ankle and lower leg.
- Grade 5: Skin ulcers with infections and inflammations, particularly in the lateral malleolus, the knob on the outside of the ankle.
- Grade 6: Enlarged chronic venous ulcers with infections, especially around the ankle.
Warning signs and symptoms of CVI
- Calf pain, especially after extended periods of standing or walking
- Leg cramping or numbness along with varicose veins
- Swollen leg or burning sensation in the leg, similar to muscle pain or muscle strain.
- Thickening of skin on the leg.
Chronic venous ulcers caused by CVI
Unlike other chronic ulcers, venous ulcers caused by CVI are specifically characterized by some distinct attributes:
- Ulcers are frequently found over bony prominences or knobs around the ankles.
- Ulcers are considerably shallow since they only involve superficial veins.
- Overtime, ulcers can be enlarged due to recurrence.
- The base of ulcer is usually red. Granulation tissue and fibrin are typically present in the ulcer base.
- Ulcers are wet with heavy discharge.
- The edge of the ulcer turns to darker color.
- Ulcers are usually painless unless infected or inflamed.
- Ulcers present with swollen or stiff ankles.
- Skin on the affected area discolors to dark brown.

Diagnosis of CVI
- Complete medical history and physical examination including arterial and venous systems
- Brodie–Trendelenburg percussion test to determine valvular incompetence in superficial veins
- Tourniquet test to determine the site of the incompetent venous valves.
- A Doppler ultrasound to measure the amount of blood flow through the arteries and veins
- Duplex ultrasound using high-frequency sound waves to check the speed and direction of blood flow in the blood vessels. As non-invasive procedure, it can evaluate how well the veins and venous valves function.
- Air plethysmography or venous occlusion plethysmography to measure pathophysiologic mechanisms of CVI, e.g. reflux and obstruction.
- Venography to identify the abnormality in the veins. Venography is an invasive prodecure in which an x-ray of the veins or venogram is deployed after a special dye is injected into a large vein in the foot or ankle.
Treatment of CVI
CVI is most treatable in its earliest stages. Several treatment options for CVI are available. However, a treatment plan primarily depends on symptoms and disease severity that might vary among individuals. Treatments options include:
- Wearing compression stockings: The most conservative approach is to wear properly-fitting compression stockings. Compression stockings with pressure gradient steadily squeeze the legs, helping veins and leg muscles circulate blood more efficiently. It is recommended to wear compression stockings at all times, except while taking a shower and sleeping at night. The benefits of wearing compression stockings are well evident as reducing pressure inside the veins, boosting circulation in the legs, preventing venous ulcers and accelerating wound healing process while alleviating cramping and calf pain. The degrees of compression can be adjusted, varying from 8 mm Hg up to 50 mm Hg, depending on the severity of the condition. In combination with wearing properly-fitting compression stockings as properly advised, basic treatment strategies involving lifestyle changes play a vital role in preventing CVI from recurring. Lifestyle modifications include refraining from long periods of standing or sitting, flexing and extending legs, feet and calves, exercise regularly (e.g. swimming, dancing and cycling), maintaining a healthy weight, keeping legs elevated while lying down and avoiding tight trousers. To facilitate blood circulation in the veins and mitigate leg pain, gentle foot and leg massage and cold compression can be applied.
- Wound care for localized chronic venous ulcers: The standard of care for localized chronic venous ulcers involves the wound dressings aiming to remove necrotic tissues or dead cells and enhance wound healing process while maintaining the wound in a moist environment. In case that the ulcers are or tend to be infected, antibiotics might be prescribed to treat or prevent infections. To prevent flaky skin that can crack easily, practicing good skin hygiene by keeping skin moisturized is very important. It is also advised to apply compression bandages as a means to reduce ambulatory venous pressure in the legs and feet, control edema and reduce blood pooling in the veins.
- Sclerotherapy: Performed under the guidance of ultrasound, sclerotherapy involves the injection of a chemical solution directly into affected veins, preventing blood from collecting in those veins. Sclerotherapy can eliminate the pain and discomfort of these veins and helps minimizing complications, such as venous hemorrhage and ulceration. Since it is a non-surgical approach, patients usually achieve a speedy recovery and a faster return to normal activities, along with cosmetic results. It is also frequently performed in combination with oral medications to help heal venous ulcers.
- Endoscopic vein surgery: If the patients do not respond to any of the treatment approaches, different types of surgery to redirect the blood flow in the veins might be considered hinging upon the causes of CVI and each patient’s conditions. In case that advanced CVI gives rise to severe swelling in the legs affecting patient’s daily life and activity, the vascular surgeon often performs the surgery that intends to extensively repair the damaged venous valves. In some cases with high severity, vein bypass surgery might be indicated, using a portion of healthy vein transplanted from elsewhere in the body e.g. the arm to reroute blood around the vein affected by CVI. If the veins are partially or completely occluded due to blood clots, surgery to remove these clots might be required, allowing for an increased blood circulation to the veins and venous ulcers. In most of the cases, if indicated, surgeries help eradicate the pathological causes of CVI and alleviate symptoms, such as leg pain and swelling, resulting in a better quality of life.
With time, the severity of CVI, along with the complexities of treatment, increases as the disease progresses. The earlier it is diagnosed and treated, the better chances of being cured and preventing serious complications. If warning signs of CVI exhibit, e.g. varicose veins, swollen legs, skin discoloration and chronic ulcers over the skin of lower extremities, immediate medical assistance provided by the expert vascular specialist must be sough before it gets too late to be fixed.











